Background: In India, we don’t see many people who are clinically obese, but almost everyone has a belly. This suggests that a significant portion of the population is overweight. So, the question arises: how do we tackle this overweight issue?
Before diving into solutions, let’s understand why we gain weight in India:
1) Overeating
A large portion of the Indian diet consists of carbohydrates (70-80%), which aren’t very satiating. This makes it easy to surpass our caloric limits. Whether it’s a glass of milk, fruit juice, sweets, or a pack of chips, we tend to consume more calories than necessary over home cooked food, even when we don’t overeat in the traditional sense. Our meals and food is full of fiber which somewhere helps us to not overeat and become obese.
2) Low BMR (Basal Metabolic Rate)
Here’s where things get more complex. People over 40 typically don’t overeat in my clinical experience and observation. It may be hard for overseas people to visualise but we have huge families, friends, and job circles that can give us a very good estimation of that specific population without looking into the data. In my training camps, i have 40 to 50 athletes coming from different cultures.
In fact, we can make two observations in India to support this:
- Most people eat home-cooked food and avoid eating out or consuming packed foods, which are often high in calories and sugars.
- People generally have three meals a day, with one snack in between. This makes it easier to calculate calories, since there’s no external junk food consumption. We don’t eat out. So we know how much we are eating. For example: I can calculate calories of any of my family members without having to talk to them. Its fairly standard. So bear with me… and read on
Now, let’s focus on weight gain. It’s easy to understand that overeating leads to weight gain, but let’s look at the low BMR issue. I believe this is where most of the problem lies, especially for people over 40—particularly women.
Weight Gain and Low BMR:
Many people are eating optimal calories for their muscle mass, height, and genetics, yet still gaining weight. Why? The issue often lies in insulin resistance, which is caused by a carbohydrate-heavy diet mixed with sugar and fat. Simply put, these individuals can’t process glucose effectively, even if they’re not overeating. This leads to lower BMR, meaning the body requires fewer calories to sustain itself. The body compensates by storing excess calories as fat. Over time, people eventually lower their calorie intake with age to match their BMR. But this only results in a plateau; they stop gaining weight but don’t lose fat either.
Typical blood report in my subjects showed High fasting glucose and high TG’s and normal cholesterol in high carb diet.
The Problem:
So how can this population lose weight if they are already eating optimal calories? They can’t simply eat less. You can’t expect someone to consume less than two chapatis per meal! This represents what I like to call the “India Dogma”—the Indian Conundrum.
The Solution:
Increase glucose uptake, improve insulin sensitivity, and eventually boost BMR.
Question: What’s the best option for such individuals in India: Ozempic or Metformin?
My answer is Metformin.
Metformin vs. Ozempic:
While both Metformin and Ozempic (semaglutide) are used to manage blood glucose in type 2 diabetes, they work in fundamentally different ways, though their end goal—lowering blood sugar—is similar.
Metformin:
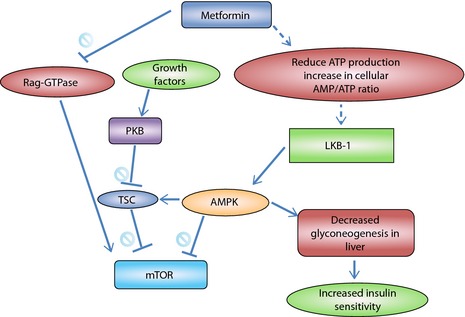
Metformin primarily targets:
- Insulin resistance
- Liver glucose production
It doesn’t directly affect insulin secretion (which isn’t a problem for most people in India with insulin resistance). Instead, it reduces glucose production by the liver and slows glucose absorption from the intestines.
Key Benefit for India: In a country with many people suffering from insulin resistance due to the high-carb, sugar, and fat – mixed diets, Metformin can help regulate glucose metabolism without suppressing appetite. But it can’t correct it! So a good strategy in my view would be adding exercising & nutrition therapy (suiting the subjects metabolism) together with Metformin to repair IR.
Ozempic (semaglutide):
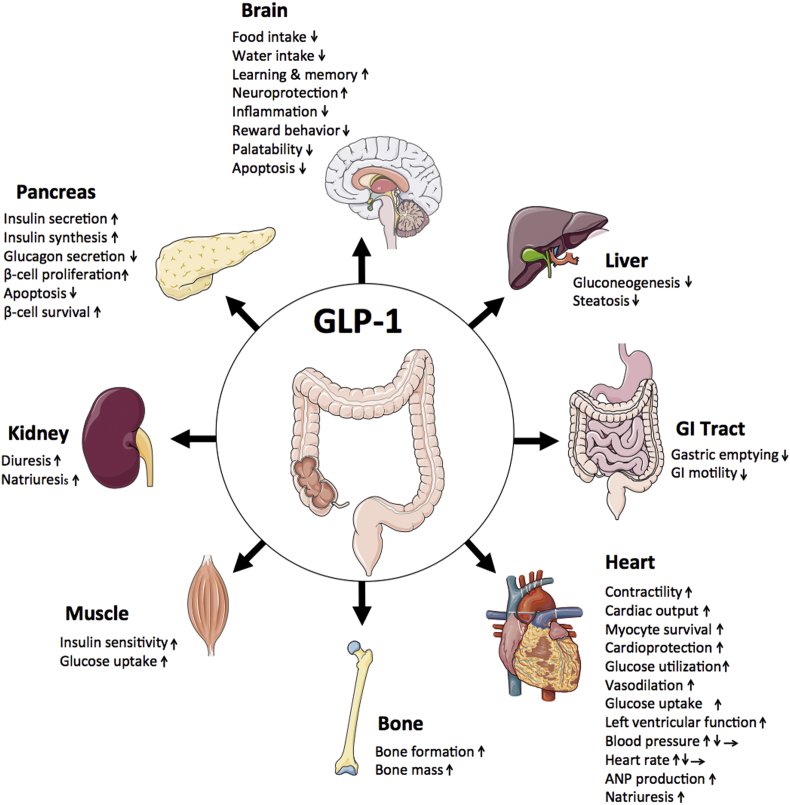
Ozempic works through the GLP-1 receptor, a hormone produced in the intestines after eating. It has several actions:
- Stimulates insulin release when blood sugar is high.
- Reduces glucagon release, which typically signals the liver to produce glucose.
- Slows gastric emptying, which leads to reduced appetite and weight loss.
- Increases insulin sensitivity through its effects on the pancreas and gut.
Key Difference: Ozempic helps control blood sugar and appetite, but its appetite-suppressing effect could be too aggressive for those who aren’t overeating but still have metabolic issues.
Key Differences:
- Mechanism of Action: Metformin targets insulin sensitivity and liver glucose production, while Ozempic mimics GLP-1 to stimulate insulin secretion, inhibit glucagon, and delay gastric emptying.
- Side Effects: Ozempic can cause gastrointestinal issues like nausea and has a significant effect on weight loss, which is beneficial for those who are overweight or obese. Metformin can also cause digestive issues but doesn’t suppress appetite.
Metformin vs. Ozempic for Different Populations:
For individuals in India dealing with insulin resistance and low BMR, Metformin would be the better choice. It targets the root cause of weight gain: insulin resistance—without suppressing appetite. For those who aren’t overeating but still have excess weight due to metabolic issues, Metformin works to normalize glucose metabolism without the risk of muscle loss, which is a major concern for many individuals over 40.
Ozempic is more suitable for those who struggle with overeating and need appetite control. For individuals who are not overeating but still have a slow metabolism due to insulin resistance, Ozempic could lead to unnecessary muscle loss because of its appetite-suppressing effects.
1. BMR and Fat Loss:
If someone’s BMR is low and they are losing muscle mass due to insulin resistance, Metformin could help by addressing the root cause of insulin resistance, thereby restoring proper glucose metabolism and preserving muscle mass.
2. Appetite Control and Fat Loss:
In individuals who are already eating sufficient calories but still not losing fat due to metabolic dysfunction, Ozempic’s appetite suppression could make things worse. It could lead to further muscle loss and nutrient deficiencies, which would hinder long-term fat loss.
3. Long-Term Fat Loss and Insulin Sensitivity:
For individuals who aren’t overeating but have insulin resistance and low BMR, the goal is to restore metabolic function without suppressing appetite. Metformin improves insulin sensitivity and glucose metabolism, supporting more natural fat loss without compromising muscle mass.
Conclusion:
For people who aren’t overeating but are struggling with insulin resistance and a low BMR, Metformin is a better fit than Ozempic. Metformin works to improve metabolic function and insulin sensitivity without the appetite-suppressing side effects of Ozempic. Metformin helps target the underlying issue of insulin resistance, making it a more suitable option for weight management in this population.
BONUS: Protein Deficiency Risk:
Since the majority of the Indian population is vegetarian, protein intake is often insufficient, leading to muscle loss. When you add a calorie deficit (such as with Ozempic’s appetite suppression), this can exacerbate protein deficiency, which further increases the risk of lean muscle loss. Given the lack of access to quality whey protein for many people, Ozempic could be harmful in this context, especially for maintaining muscle mass.
Thus, Metformin is a more practical and sustainable option for improving metabolic health in India unless somebody is not able to control their hunger, overeats, and is obese. This population as I said is far less comparitively.
For more insights, check out my podcast: